At 7 p.m. on a Saturday in April, Marc Schiffman, still in hospital scrubs, was standing in line to pay for a few children’s walkie-talkie sets at a Target in Harlem. Customers around the store began to clap in honor of healthcare workers, a new custom of the COVID-19 era. Customers approached Schiffman to thank him for his service and ushered him to the front of the checkout line.
The walkie-talkies, originally designed for kids by a company called Relay, were for patients. Schiffman and his colleague Tamantha Fenster, an obstetrician and gynecologist at New York Presbyterian Weill Cornell Medicine, were trying to devise a low-cost way for families of COVID-19 patients to communicate with their loved ones in intensive care. Video chat was proving to be too depressing for families and too time-intensive for nurses. Walkie-talkies had the potential benefit of letting family members talk to a patient whenever they wanted without the help of a nurse.
“It’s basically a speaker that connects to an app,” says Schiffman. That weekend he and Fenster gave out the Relay walkie-talkies to a few patients and told their families to download the Relay app, which would let them speak to the patient just by pressing a button. The families loved it, and by Sunday afternoon, Schiffman and Fenster had made contact with Relay and convinced the company to waive the walkie-talkie’s monthly subscription fees for its patients. The experiment to connect COVID-19 patients with their families has now blossomed into a new hospital program called the VoiceLove Project that has the ability to connect patients in all kinds of circumstances with their family. So far, the Relay devices have been deployed across 10 care units at New York Presbyterian, reaching dozens of patients.

Keeping isolated patients connected
Many doctors, like Fenster and Schiffman, haven’t been able to serve on the frontlines of COVID-19. But in some instances, like this one, that’s given them the space to solve for some of virus’s less catastrophic impacts.
In April, Fenster got word that she would be needed to assist in the hospital’s intensive care unit. COVID-19 cases were rising to their peak in New York City and the hospital needed everyone on staff to help out. Fenster had never worked in the ICU, so she spent weeks interviewing colleagues and studying intensively in preparation. New York Presbyterian ultimately was able to get intensive care doctors from around the state to come down and work in critical care, obviating Fenster’s new role.
“As a physician, there’s a sense of peace and fulfillment in being able to help and do something and being told I was no longer needed fill the role of an ICU doctor—I couldn’t accept that,” she says.
She convinced Schiffman, a radiology specialist who primarily conducts minimally invasive surgeries for cancer and other vascular illnesses, to brainstorm with her about how they could help patients suffering from COVID-19. They began going on rounds with ICU doctors. It quickly became apparent that doctors needed someone who could call patients’ family members with updates. Patients weren’t able to have visitors, because of the risk of COVID-19 transmission, so doctors could not confer with families in person. With critical cases mounting, doctors or nurses were increasingly strained as they tried to address overwhelming patient needs as well as keep loved ones informed. In response, Fenster started a program called Critical Care Connect to ensure that someone was reaching out to families daily.
“The idea behind it was: the same physicians every day, calling the family members at the same time, so they can have some reliance,” she says.
Families were grateful for the contact, she says, but what they really wanted was to talk to their sick family member. Patients with severe COVID-19 often have trouble breathing, so much so that a tube is inserted into their trachea to bring more air into the body. After patients are intubated, as the procedure is called, they can’t speak for as long as the tube is in place. This puts family in a complicated and desperate position. They cannot see their loved one in person, they cannot speak with them, and they must live with the anxiety that they might die at any moment.
Tamantha FensterThey said, please, if they could just hear our voice.”
“They said, please, if they could just hear our voice,” says Fenster. To give family more time with the patient, nurses were holding up iPhones and iPads to facilitate video chats so families could get a better sense of how their loved one was doing. But this scenario introduced new problems. For one, it was increasing nurses’ exposure to sick patients, which put them at additional risk. These added visits with patients also required additional personal protective gear at a time when supplies were limited. Furthermore, the videos of patients sedated with tubes coming out of their bodies were disturbing to family members.
“We had family members actually tell us, please don’t show us that video again,” says Fenster.

A new use for a kids’ walkie-talkie
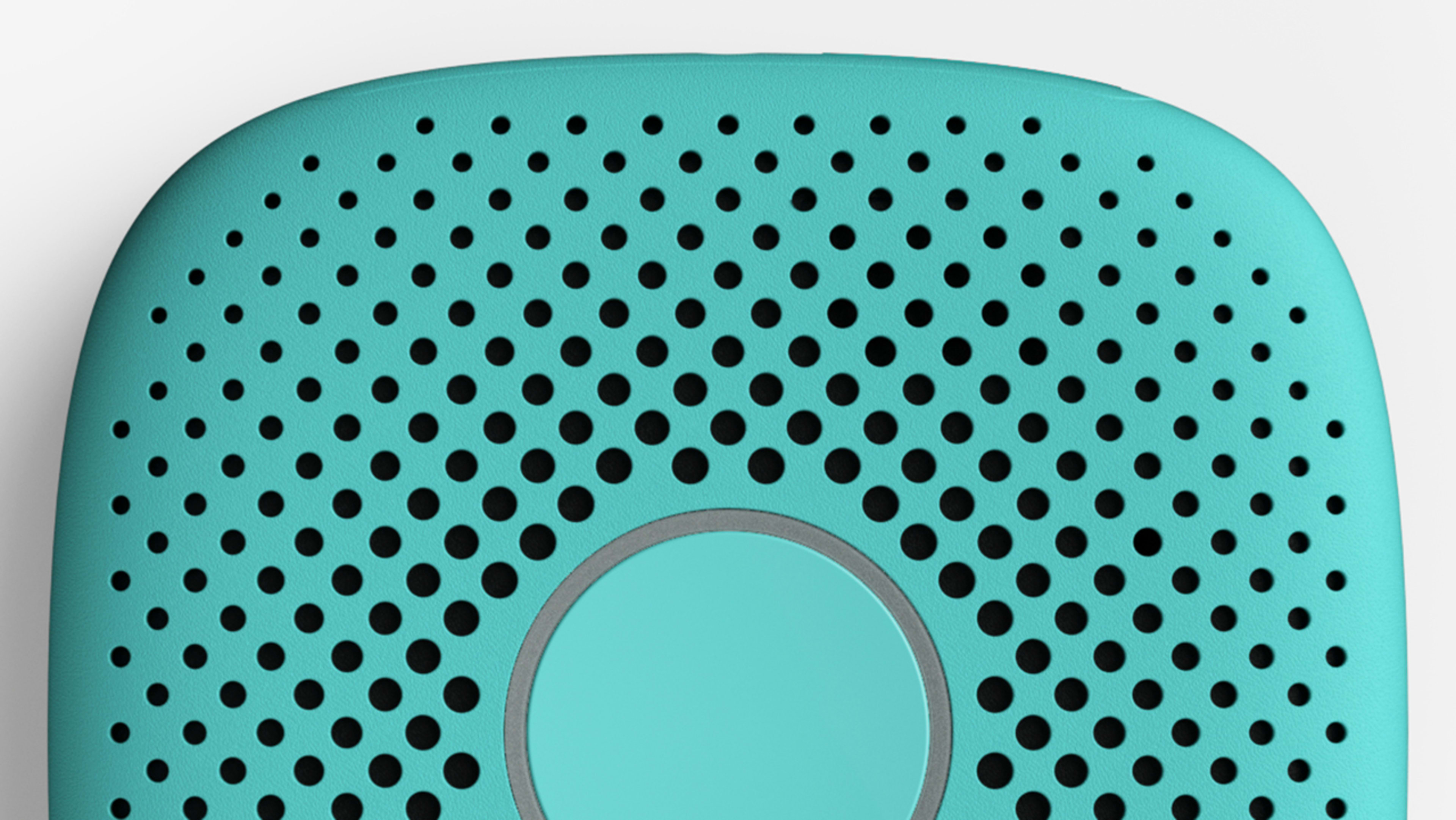
She and Schiffman started brainstorming possible alternatives. The idea of walkie-talkies came up. A two-way radio was promising because it didn’t introduce the complications of video or a phone. After much searching around the web they found the Relay walkie-talkies. The device is a small square speaker with a button at the center. Because it was originally built for kids, it has a simple design. All you have to do is press the button to talk to the person on the other end.
“It’s basically designed for parents who don’t want their kids to have a smartphone because of all of the apps and all of the risks that come with that,” says Schiffman.
At New York Presbyterian, the little speaker proved to be a hit with families. They would get on the speaker to share a random memory or a fleeting thought—maybe a joke. They were calling just to talk, knowing that their loved one was on the other end of the line, whether they could respond or not. The beauty of the Relay speaker in this particular context is that a patient can get a message without touching a thing. It can also be used by multiple people. For example, if a patient’s family knows that the patient would like to hear from a minister or rabbi, that religious leader can download the app and make contact with the patient. There are still other advantages to this simple device. If the patient is able, they can press the big button on the speaker and talk back, like a regular old walkie-talkie. If a nurse thinks a patient needs quiet, the device can also be shut off.
Because the Relay walkie-talkie was never designed for medical purposes, Schiffman and Fenster have created additional elements to make it more hospital ready. Fenster reached out to Mitchell Tung, an industrial designer and friend of hers from college, to see if he could help design a casing for the device that would keep it from getting contaminated and allow it to be attached to a hospital bed. The result is a little velcro-backed white clam shell that fits around the device and can be tossed out and replaced as needed.
Both Fenster and Schiffman hope the device and casing can be a model for other hospitals, though Weill Cornell Medicine owns the intellectual property related to the clam shell. They also think the Relay could be a good fit for nursing home residents, some of whom suffer from neurodegenerative diseases like Alzheimer’s. While families have responded well to the Relay, there’s no data on how listening to family members over a speaker will affect patients. While Schiffman says that it’s well understood that interactions with family are generally good for patients, he and Fenster are currently applying for grants to study the device’s impact on stroke patients and patients in a coma.
“It’s funny because initially we were talking about all these sophisticated walkie-talkie things and then we come upon this children’s device,” says Fenster. “The simplicity of it was actually one of the best things, because if you did have someone who had Alzheimer’s or, you know, had just woken up and was very weak, there’s no thought involved. It’s just one button that they have to push.”
Recognize your brand’s excellence by applying to this year’s Brands That Matter Awards before the early-rate deadline, May 3.