In a lab at Rice University in Houston, a tiny 3D-printed model works like a part of a human lung: When air is pumped into the model, red blood cells take up oxygen as they flow through 3D-printed blood vessels.
It’s a step toward a future when patients who need an organ donation could have an organ bio-printed from their own cells instead of sitting on a waiting list. There are currently more than 100,000 people waiting for a lifesaving transplant in the U.S. alone, and those lucky enough to get a transplant face a lifetime of medication to prevent organ rejection. Researchers have been exploring the idea of 3D-printing organs since the early 2000s, but one of the key challenges has been how to create the networks of veins and capillaries that flow through organs to keep cells alive. The new process used to make the lung-like model is one way to solve that problem.
“What we’re trying to do is make complex vascular architecture, because we know that most of the organs in the body–the solid organs, the ones that are most critically needed for transplant–are crucially supported by blood vessel networks,” says Jordan Miller, an assistant professor of bioengineering at Rice University’s Brown School of Engineering and one of the authors of a study about the new bioprinting technology. A lung needs airways and blood vessels; a liver needs bile ducts and blood vessels.
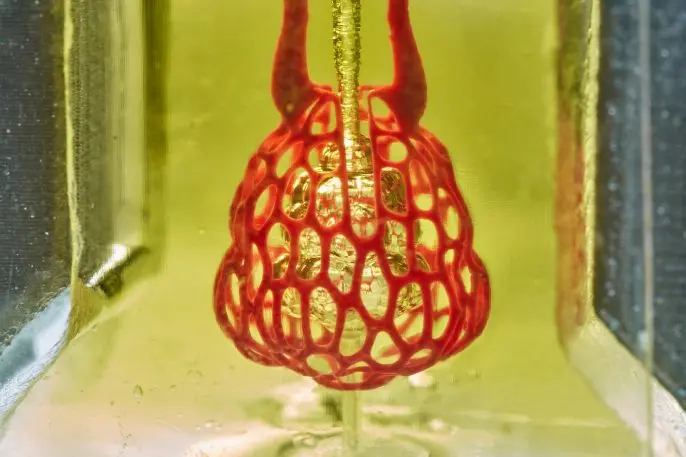
The researchers tested printing implants for liver disease, which they implanted in mice with liver injury; the mice survived. They worked with Nervous System, a Boston-based design firm, to design the lung-mimicking structure. Two networks of blood vessels surround an airway, and as the airway is rhythmically inflated and deflated to “breathe,” the blood becomes oxygenated. The design firm is creating software that scientists can use to design customized, complex structures with multiple vascular networks.
“Our work is about creating new tools and methods that take advantage of the possibilities of digital fabrication and computation,” says Jessica Rosenkrantz, cofounder and creative director of Nervous System. “Traditional design software doesn’t allow you to make the sort of structures that reflect the complexity we see in nature. The generative design tools we create at Nervous System open up new ways of “growing” structures with the intricacy and level of customization needed to engineer living tissues.” Ultimately, she says, it might be possible to 3D-print lungs that perform better than the real thing. “I think the real challenge is, can we design something more efficient than human lungs? Can we use 3D printing not just to reproduce the native structure, but think about ways to make lungs that work better?”
It will take time before bioprinted organs are used in transplants, but it’s likely to happen. “I believe that bioprinting is going to be a major part of medicine within the next 20 years,” says Miller. The researchers are now beginning to work on 3D printers that are larger in size and higher in resolution so that it’s possible to print even more complex structures. (In the liver, for example, where there are more than 1 billion functioning cells calleed hepatocytes, it will be necessary to build bigger, more intricate structures to support all of those cells.) The researchers are also sharing open-source designs for their printer so others can also use it to get closer to the goal of a fully functioning organ.
Recognize your brand’s excellence by applying to this year’s Brands That Matter Awards before the early-rate deadline, May 3.