This article is about one of the honorees of Fast Company’s Next Big Things in Tech awards for 2022. Read about all the winners here.
In 2016, Trevor Martin, a biology Ph.D. at Stanford, was growing restless. He’d fallen in love with synthetic biology, where discoveries were being made weekly, but was frustrated with the lab’s distance from real-world applications. And among the new discoveries, nothing was as tantalizing as CRISPR, a genetic tool found in bacteria and other organisms that researchers were using to effectively cut and paste DNA. If anything in a lab could help people—with anything from detecting and treating cancer to curing genetic diseases to building climate-resilient agriculture—this was it.
“Being able to reproducibly and reliably change the code of life, DNA and RNA, has been historically so incredibly difficult,” he says. “If we can program biology the same way we program a computer, that’s transformative.”
He’d been intrigued by a new paper from the lab of UC Berkeley professor Jennifer Doudna, whose pioneering research on CRISPR had been making waves, so he sent her an email. To his amazement, she responded. Martin connected with two of her star grad students, Janice Chen and Lucas Harrington, who were researching newer versions of CRISPR, including one that reported on the presence of targeted genes. In 2017, the four of them launched Mammoth Biosciences in a small lab in San Francisco’s Dogpatch neighborhood, with the aim of turning CRISPR’s pair of molecular scissors to a whole suite of apps. “We can leverage the great foundation that’s been built and take CRISPR to the next level,” says Martin.
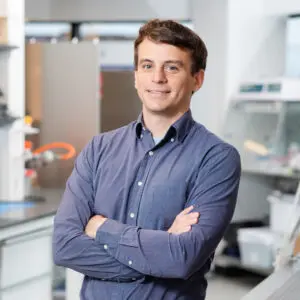
The goal is to build a CRISPR “platform” for the masses, including a diagnostic “search engine” for diseases, and permanent cures for those diseases, by eliminating or actually changing the genetic mutations behind them. Now 190 people large, the company has since expanded to a glassy headquarters in the south of San Francisco, and has raised $195 million from investors including Alphabet’s Verily, Amazon, Grail founding CEO Jeff Huber and Apple’s Tim Cook, valuing the company at over a billion dollars. Mammoth “will be completely unignorable in terms of the transformative impact it can have on patients’ lives,” Martin, now Mammoth’s CEO, says matter-of-factly.
Getting CRISPR in the body, and beyond the liver
In just a decade, CRISPR has rewritten the paths of a generation of scientists, sent dozens of companies on a gold rush, sparked a dramatic patent battle, and earned Doudna and her collaborator, Emmanuelle Charpentier, the 2020 Nobel Prize. Clinical trials, meanwhile, have shown promising results for using CRISPR to cure blood disorders such as sickle cell anemia. Researchers have begun applying CRISPR to develop cures for any number of ailments: cancer, congenital blindness, AIDS, type 2 diabetes, maybe even neurological disorders like Huntington’s disease.
The technology is also finding uses beyond sick patients: making tweaks to plants in order to help them adapt to a changing climate; helping bodies accept lab-grown organs; curing malaria in mosquitoes, which could eliminate the disease in humans. There are more thrilling and risky prospects too, like germline genome editing to build disease-resistant designer babies, or using CRISPR to resurrect the woolly mammoth.
Martin says the company’s name “is a bit of a cheeky play” on that Jurassic Park-ish idea. But it’s really meant to reference the company’s ambition.
One of Mammoth’s major goals is getting its therapeutics in the body, in vivo, and beyond cells in the liver—thought to be the easiest target for clinical uses—into other cells where diseases originate. Getting CRISPR to work within the body is “where the field has the biggest challenges and where you can really unlock the most value for patients,” he says.
The problem is that the conventional CRISPR tools—specifically the associated Cas9 protein, the molecular scissors that cut DNA—are too big to fit inside the delivery systems that can target certain cells inside the body. Instead, Mammoth pursued Cas proteins—in the Cas14 and Casɸ families—that are smaller, possibly more efficient, and potentially more effective than Cas9. These “ultra compact” enzymes measure down to a third of the size of Cas9, which means they can fit into the commonly-used adeno-associated virus and, according to early data, the lipid nanoparticle technology used to get mRNA-based COVID-19 vaccines into cells.
At first, the more compact enzymes were met with skepticism. “People didn’t really think that these would work, or that they weren’t possible,” Martin says. It helped having scientists leading the company. “That just creates a very different culture, knowing the scientific risks, when to push it forward and to really understand what’s the right direction,” says Martin. After publishing a 2018 paper, Mammoth licensed a family of Casɸ proteins from UC Berkeley, where a team including Doudna published research about them in February 2020 in Nature in July 2020 in Science. “We’ve shown [the smaller Cas enzymes] are incredibly effective.”
Alongside an internal pipeline, it’s striking deals to build out its CRISPR toolkit. A COVID-19 test developed with Agilent, the DETECTR BOOST, combines the accuracy of a PCR test with the speed of an antigen; in January it became the first CRISPR-based high-throughput test to be granted emergency use authorization by the FDA. In January, Mammoth also earned funding from DARPA to develop a point-of-care test that could detect up to 10 pathogens at once, and a larger, lab-based test that could detect up to 1,000. In partnership with Vertex Therapeutics, it’s developing in vivo gene-editing therapies for two undisclosed genetic targets, and is collaborating with Bayer to develop CRISPR therapeutics, in part for liver diseases. (Both companies paid around $40 million, and royalties from the two tie-ups could reach $1.6 billion.)
Mammoth is also pursuing trickier, “CRISPR 2.0” techniques, like base editing and epigenetic editing. Its COVID-19 test uses Cas12 enzymes to detect single nucleotide polymorphisms (SNPs) in the novel coronavirus spike gene—no easy feat. These tiny, single “letter” mutations are linked to disease, bacterial and viral infections, and cancer. “Not only is this very sensitive and specific,” says Martin, “but it can also be specific at the level of single SNPs. So that opens up a whole new world as well of genetic medicines and oncology and similar applications.”
Despite the software analogies, CRISPR hasn’t proved to be exactly as precise as a word processor or a code compiler, and will likely never be that accurate. Doudna, who is also a cofounder of the publicly traded CRISPR company Intellia Therapeutics, recently told the Boston Globe that base editing “works very well in research settings,” and could be effective for disrupting genes. But she doesn’t think it’s yet precise enough to correct mutations. Base editors often edit other letters too, so “you end up usually getting more editing than you might want.”
The Mammoth team—with Doudna’s expertise—isn’t deterred. Smaller Cas enzymes could make room for additional elements that can be used to better control editing outcomes. “Having ultra compact systems is even more important, because you have all this other machinery you’re trying to fit in,” Martin says. Machine learning and a high-throughput wet lab also helps. Still, “there’s no free lunch in engineering.”
Staying out of trouble
Mammoth’s ultra-compact approach to CRISPR saved it other headaches. A few months after Doudna and Charpentier’s breakthrough, scientists led by the Broad Institute’s Feng Zhang and, separately, George Church of Harvard used CRISPR to edit the genomes of living human cells in lab dishes. A vicious patent battle ensued in the courts, and this May the U.S. finally awarded the patent for the eukaryotic version of Cas-9 to the Broad Institute, not to the University of California; Doudna’s team was awarded a patent for a similar method in bacterial cells.
Martin says that avoiding that drama is “one of the reasons why of course many partners want to partner [with us], and that’s a very unique position to be at in the CRISPR space, to actually be separate from a lot of that.”
Provided patents don’t inhibit valuable science, Martin says intellectual property helps secure the money needed to do ever-costly research and clinical trials. (The company has patents for some of its uses of CRISPR.) One big question for Martin is “how do we incentivize investment so that we can have these amazing cures and diagnostics for everyone’s benefit?” This is why he wanted to work in biotech. “That’s the core of it right?”
As the investment pours in, there’s another big question for Martin’s company: What to focus on next? A new therapeutic, a diagnostic target, agriculture? It’s even harder to choose, he says, “when you have an opportunity to do anything.”
How about a mammoth?
He laughs. “No comment.”
Recognize your brand’s excellence by applying to this year’s Brands That Matter Awards before the early-rate deadline, May 3.
