Throughout the history of modern surgery, training has been accomplished as a one-to-one apprenticeship in the operating room. High-volume surgical training programs offer the best opportunities to see surgery and experience rare cases. But the challenge is most surgical training programs only take a handful of applicants per year.
For instance, Seattle’s University of Washington Department of Neurological Surgery, where I work, only takes three applicants per year for its seven-year training program. Residents learn the full breadth of neurosurgery subspecialities from 20 faculty members in 5 facilities: vascular, skull base, tumor, spine, functional, trauma, and pediatrics. With about 7,000 operations a year across our entire training program, our residents graduate having participated in 2,000-3,000 operations beginning as observers and later as assistants.
Neurosurgery is a good example of how location, size, reputation and available training slots dictate the spread of surgical knowledge. As the demand for surgery grows and our ability to save lives continues to progress, a limiting factor is the availability of highly qualified surgeons, especially in rural areas of the US and underserved areas of the world.
The era of COVID-19 has seen a rapid evolution and acceptance of telemedicine for primary care and even specialty work like mine. I see about 95% of my pediatric neurosurgical patients via telemedicine as we discuss their symptoms, pathology, and potential surgical interventions. It works surprising well and has lowered the burden of care for many families for whom taking off work or traveling to see the doctor is a huge and costly proposition, especially if it needs to happen repeatedly.

A new approach to surgical training
Just before the start of 2020, a talented colleague in Adelaide, Australia, Dr. Xenia Doorenbosch, asked me if I would proctor her through a surgery I had become an expert on over the years. The operation is called a selective dorsal rhizotomy (SDR), where the surgeon carefully cuts select nerves that come off the spinal cord to treat a condition common in children with cerebral palsy called spasticity (high muscle tone). Patients who undergo this surgery can walk better afterwards and live more independently without the profound physical constraints they had before. It is one of my favorite operations because it is so incredibly life-changing for the kids and their families.
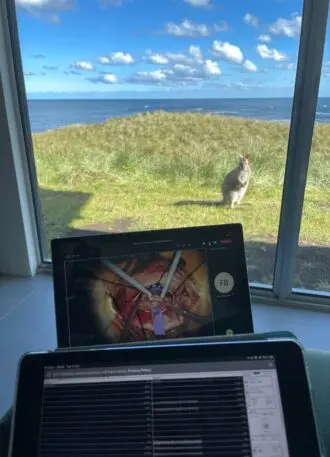
From my Seattle office, I watched a live feed from the operating room microscope in Adelaide over Teams. I talked back and forth with Dr. Doorenbosch and made suggestions as I saw the procedure unfold: “I’d cut that. Maybe leave that nerve alone. Typically, I’d take a little more over there.” It was as if I was in the operating room providing guidance. There were moments when I instinctively reached out to grab an instrument only to realize I was halfway around the world. The software I always associated with business meetings was allowing my team to guide our Australian colleagues through their first SDR procedure, in real-time, 18.5 time zones apart.
After six hours of surgery, I went home and had dinner with my family. My two kids were wholly unimpressed with my day, as they had just video-chatted with their grandparents and cousins in Florida. But for me, it was a completely pivotal experience. Imagine the ability to take expert surgical knowledge and share it with colleagues and trainees anywhere in the world on-demand or real-time, live in the moment.
Surgical training goes virtual
While being present via telesurgery is new and novel, we can expect the evolution of this experience will happen quickly. The scenario goes like this. You are early in training, you want to learn how to take out a herniated disc in a patient’s lumbar spine. You don a VR headset, pull up the case from a library to first watch the operation being done from the surgeon’s perspective. Commentary and annotations of the anatomy are overlaid for your learning and you observe the procedure from cut to skin closure. The learning surgeon advances through a virtual anatomy environment with realistic surgical instruments deployed in the scene. It’s no different than what pilots do today in simulation training: Simulate before you go live.
Telemedicine is rising, and while it’s still early, telesurgery will grow allowing the democratization of surgery through access to training, mentorship, and dissemination of surgical knowledge. The ability to train repeatedly on real cases, on-demand will expand access to surgery and improve training world-wide. The sooner we enable the digital evolution in the operating room and empower surgeons with technology the better.
Recognize your brand’s excellence by applying to this year’s Brands That Matter Awards before the early-rate deadline, May 3.
