Months into the pandemic, there are still so many unknowns about COVID-19. Does age or ethnicity affect how likely a COVID patient is to be admitted to the ICU? Are patients who don’t enter the ICU more likely to end up back in the hospital later? And do comorbidities—other health conditions, such as diabetes, asthma, or heart disease, that may worsen someone’s COVID-19 case—have any affect on how long a coronavirus patient is hospitalized for?
A new website called COVID19questions.org hopes to answer these questions, and more, based on real patient medical record data from more than 200 hospitals. The site was created by a research consortium of 12 hospital systems, including UC San Diego Health and Cedars Sinai Medical Center, called Reliable Response Data Discovery, and funded by the Gordon and Betty Moore Foundation.
“A new disease is always difficult because you discover new things, and then you want to compare with other patients,” Ohno-Machado says. “For example, mortality in the ICU—what is it compared to other respiratory conditions? So it’s important to have available data to consult.” COVID19questions.org can draw from data on more than 59,000 patients who tested positive for COVID-19 and 29,000 who were hospitalized with the infection, to make those kinds of observations.
To protect privacy, patient-level data is never transmitted out of the individual health systems; only the data aggregates that answer a question. This way, there are no issues with privacy, Ohno-Machado says.
Clinicians, researchers, patients, and the general public are welcome to submit questions to the website. Those questions are then translated into a code that queries the electronic medical records. After each health system has run the code on their own patient records and provided the results to the consortium, its members will do a quality-control check, to make sure there weren’t any errors with maps or how that code was applied, and then post the answers to the site.
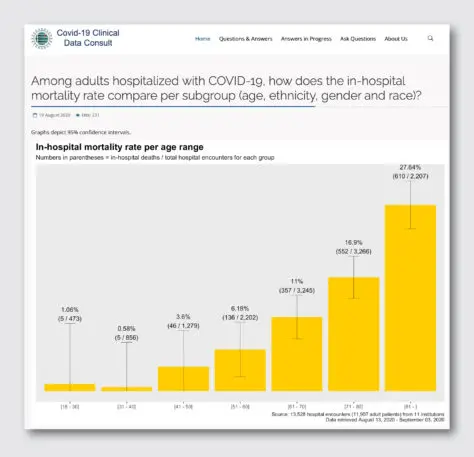
Because the answers are displayed as data, and not written-out conclusions, Ohno-Machado says there is some health and data literacy needed to interpret the results. The answer for the question “Among adults hospitalized with COVID-19, how does the in-hospital mortality rate compare per subgroup (age, ethnicity, gender and race)?” shows bar graphs that display mortality rates by each category. The biggest differences were among age groups: more than 27% of patients 81 and older have died while hospitalized for COVID-19, while only 3.6% of patients 41 to 50 did.
The graphs on mortality per ethnicity and gender indicate that more non-Hispanic people and more men have died in hospitals from COVID-19, but when you adjust each of those categories for age, Ohno-Machado says, there’s no difference in mortality along those other groups. That’s explained by an adjusted analysis below those graphs, but it might not be immediately clear to some readers that age is the most important factor for mortality. (The site does lay out considerations readers should take when interpreting the answers.)
Still, the consortium hopes this site makes this information more accessible to the public than when only scientists can ask questions, analyze data, and publish their results in academic journals. The site isn’t meant to replace clinical studies. The site won’t answer questions about remdesivir, for example, because there are clinical trials already researching that.
Instead it aims to answer things there would never be a clinical study on, such as the rate of readmission for patients who never went to the ICU. Hopefully, Ohno-Macado says, these findings can complement the clinical trials, and give us a better understanding of COVID-19. “Some things will never be subject to a randomized control trial, they’re just observations,” says Ohno-Machado.
Recognize your brand’s excellence by applying to this year’s Brands That Matter Awards before the early-rate deadline, May 3.