The coronavirus crisis has turned life as we know it upside down. Since March, millions of people have been sheltering at home without a clear answer regarding when life will resemble something close to normal again. We’re consequently experiencing an unprecedented level of widespread anxiety. At Brightside, the telemedicine service I cofounded to provide expert care for depression and anxiety, we’ve seen a 50% surge in new members seeking mental health support. Countless people are wondering if the discomfort they’re experiencing is “normal” or if others are in the same boat.
Not only is the feeling normal given the circumstances. It has a name: adjustment disorder. Clinically speaking, adjustment disorder is a stress response syndrome people experience in light of an identifiable life stressor (loss of a loved one, job, or home due to a natural disaster, etc.). In the absence of a catastrophe, generally around 1% of the population experience it. The COVID-19 crisis has challenged our notions of what to expect from our lives, our routines, and the core institutions in our society. Many of the things we cherish and value now seem more fragile than we imagined.
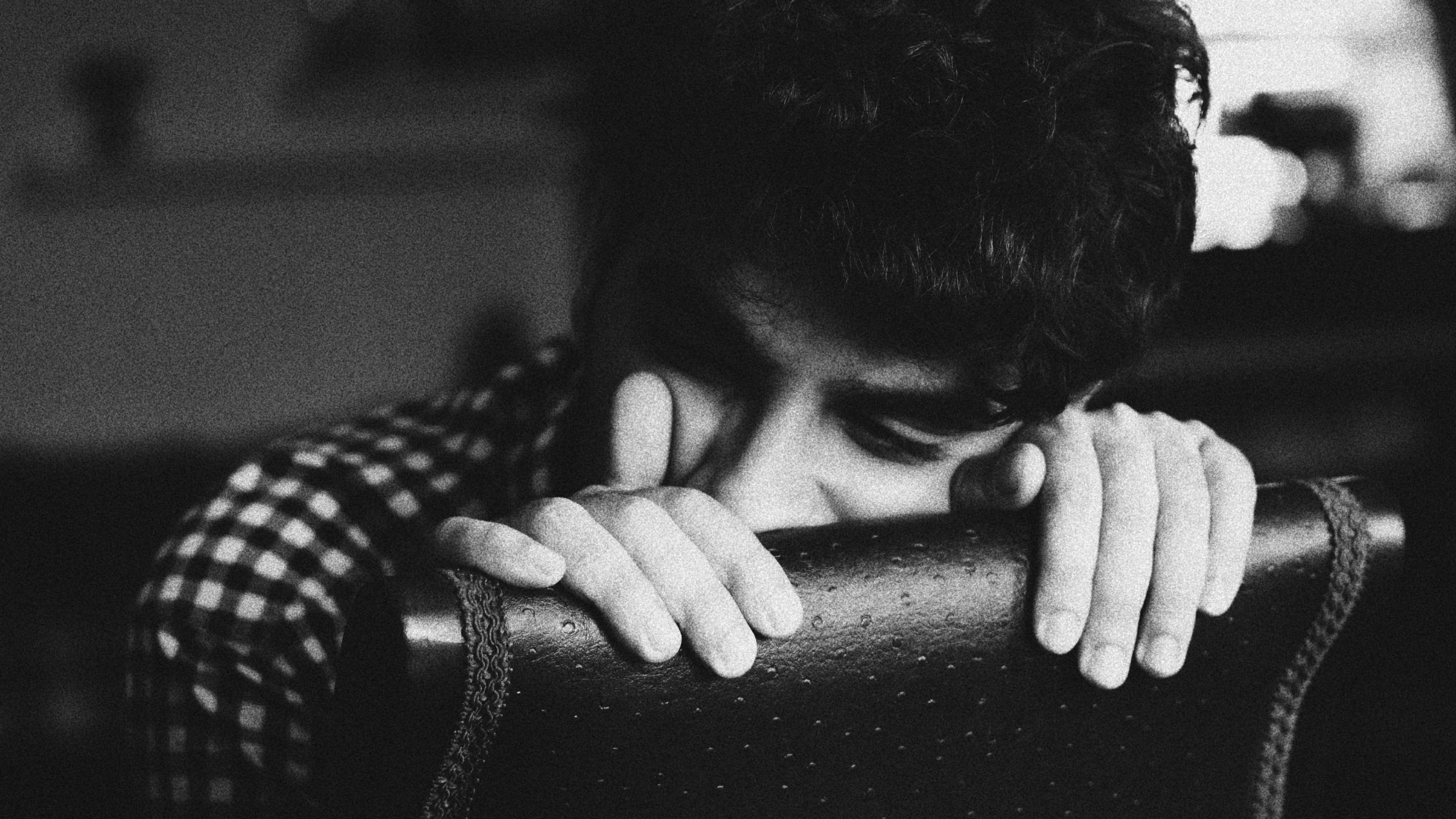
The number of people experiencing adjustment disorder has likely skyrocketed, with people suffering from heightened anxiety, a depressed mood (often called situational depression), and trouble focusing on work or school. In the worst cases, it can also increase the risk of suicidal ideation and substance abuse.
If this sounds like something you’re experiencing, you might be asking yourself a few questions. How long will it last and what can you do to feel better? Is professional treatment necessary? How can it be safely accessed from home? Or, if you run a company, how can you help your team weather this storm? Let’s dive in.
Symptoms and timelines
Symptoms of adjustment disorder typically start within three months of the stressful incident. They can feel a lot like depression and anxiety, and in some cases evolve into more full-fledged cases of mental health disorders (more on that later). In addition to the symptoms outlined above, you may notice that you no longer enjoy things that used to bring pleasure, or experience trouble with sleeping or appetite, or find yourself avoiding important tasks more often than usual.
Typically, symptoms last no longer than six months after the stressful event. However, chronic adjustment disorder can persist, especially if what’s causing it is ongoing, such as unemployment, illness, or in our case, many of these factors combined within a global pandemic. Acknowledging symptoms early, and creating a plan to tackle them head-on, can help avoid prolonging the symptoms or have them evolve into clinical depression or anxiety.
What you can do to feel better
For the majority of people experiencing adjustment disorder, symptoms will be temporary. Unlike clinical depression, which does not require a reason or stressful life event to be associated with it, what triggers adjustment disorder will, in most cases, eventually come to an end. Timelines related to COVID-19 remain uncertain, which exacerbates the anxiety associated with it. But reminding yourself that we will get to the other side of this can greatly help your mental state.
Addressing your feelings is also helpful. When I am working with patients, I ask people to name the emotion they’re feeling. This seems simple, but categorizing the feeling can be very helpful. If there’s something specific you are worried about, hit the play button and imagine how that worry plays out. If there is something you can specifically do to alleviate it or avert it, then act on it. If it is out of your control, it is probably best to distract or sublimate with a soothing activity—exercise, a walk in fresh air, stretching, a warm bath, cooking, art projects, etc.
If money is a concern, creating a budget, researching local food banks, or applying for unemployment may all be useful tactics. Random fears about whether schools will reopen in the fall or worrying about when we will have a vaccine is unlikely to be something you can act on if you are not a school administrator or a virologist. So, distraction or sublimation is best put into play as a coping mechanism.
How you can help others (and your team)
The social stigmas associated with mental health issues have prevented people from discussing their struggles—and seeking help for them—long before COVID-19. The isolation that many people now find themselves in can exacerbate this phenomenon. For many, opportunities to talk about their feelings have all but vanished. The good news is that with COVID-19, we are alone, together. Even though we may be physically isolated, we are in this together in that it is affecting all of our fellow humans, so it’s more important than ever to connect with others, even if you personally feel okay.
If you think an employee, teammate, or friend is struggling, the easiest thing you can do is check in on them. Make it clear they have a safe space to talk candidly about how they are doing and what they are experiencing. Don’t confuse this with a suggestion to interrogate them about their mental health. An open-ended “How are you doing with all of this?” can disarm whatever is holding them back and make them feel more comfortable opening up.
If you’re an employer, the best thing you can do is address the mental health implications of what we’re all going through in the open for the entire team to see. You might even share this post so they know what adjustment disorder is. If you aren’t already regularly holding all-hands meetings to keep the team engaged, it’s a good time to start. Mentioning the topic of mental health during those meetings can be helpful. If it’s feasible for your business, providing mental health services, or at least resources, to your staff is a good idea. Revisit your employee assistance programs to make sure you’re offering all that you can when it comes to mental health.
How to know if you should seek professional help
In the same way that we don’t know how many asymptomatic coronavirus carriers there are relative to those with frank illness, we also don’t know if adjustment disorder is the larger iceberg lurking under the water’s surface. Among those struggling with adjustment disorder, some percentage will progress into real illness, which will manifest as clinical anxiety or depression.
When symptoms start to interfere with your ability to work or practice self-care, or important relationships in your life, it’s time to consider speaking with a professional. If you’re unsure how severe your symptoms are, taking a clinically validated screening tool is a useful way to score them. You can find these for free online—we have one available on Brightside.com and will provide recommendations based on your symptoms and scores.
The silver lining of COVID-19
It’s hard to think of a time when this many people were feeling as introspective as they are now and looking for ways to talk about it and feel better. Paying attention to mental health is extremely important, and it seems we’re finally hitting a tipping point of acceptance.
There’s a lot of uncertainty related to COVID-19, but the truth is life has always been uncertain. This period has not only given us an intense boot camp in resilience; it has also provided an opportunity to ask ourselves what really matters. All of us have thought about what we’ve missed most during shelter-in-place, but it has also reframed exactly what we actually need to be happy. When thinking through what your new normal might look like, you might want to evaluate which parts of your old normal you might like to leave behind. You may never have such a clear opportunity to do so again.
(If you are having thoughts of suicide, call the National Suicide Prevention Lifeline at 1-800-273-8255 (TALK) or go to SpeakingOfSuicide for a list of additional resources.)
Dr. Mimi Winsberg is cofounder and chief medical officer of Brightside, a mental health telemedicine service.
Recognize your brand’s excellence by applying to this year’s Brands That Matter Awards before the early-rate deadline, May 3.